Great article on a subject very close to all of our hearts.
WHATS IT ALL ABOUT?
This was a large survey, conducted from 2 points of view – a point prevalence spot check, as well as a realtime survey in 51 UK ICU’s. It would hopefully give us some insight into what we are all up to with our patients and at the same time, as ICNARC are so good at, provide some benchmarking for practice.
ICNARC was commissioned by the National Institute for Health Research Health Technology Assessment Programme to design and conduct a study to establish current sedation practice in UK adult critical care. The overall aim of the study was to provide baseline data on current practice to inform evidence synthesis and potential future primary research. Specific objectives were to establish:
- Report current sedation practice
- Point prevalence study (PPS) in a representative sample of UK adult general critical care units, the current prevalence of use of sedative agents and regimens.
- Reported Vs observed clinical practice

HOW DID THEY DO IT
Databases were interrogated to capture information on management of sedation, as well as the use of specific sedative and analgesic agents. With respect to analgesia, the focus was on analgesic agents with a sedative effect, such as intravenous opioids, rather than on oral or regional analgesia. For patients who were on the units >24hours:
- Numbers (percentages) of sedated patients were reported.
- Those considered for and/or receiving a sedation hold were reported
- The number (percentage) of patients receiving each sedative and analgesic and combinations of agents during the previous 24 h were reported
- For agents received by five or more patients, the mean (SD) of the highest rate of infusion (in milligrams per hour) and the total dose (in milligrams), including both infusions and boluses.
- The proportion that received the unit’s reported first-choice sedative agent was summarised.
- Same for analgesics
WHAT IT FOUND
NATIONAL SURVEY
Sedation
- 57.0 % of units reported having a written sedation or sedation/analgesia protocol.
- 23.0 % of these reported that compliance was routinely audited
- 93.9 % reported routinely using a sedation scale/score to assess the depth of sedation
- 64.7 % reported using the Richmond Agitation-Sedation Scale (RASS) and 24.9 % reported using the Ramsay Sedation Scale (RSS)
- 93.9 % reported that a sedation hold was considered daily for patients
- 47.3 % reported routinely auditing compliance
- 93.3 % reported using the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU)
- 98.1% of units used propofol as 1st agent
- 88.3 % reporting that propofol was generally their first choice of sedative agent
- 32.2 % of units reported very frequent use of midazolam
- 6.1 % reporting midazolam (three units reported both agents)
- 32.7% used clonidine as alpha-2 agonist of choice
- Only 10.3 % used dexmedetomidine
Analgesics
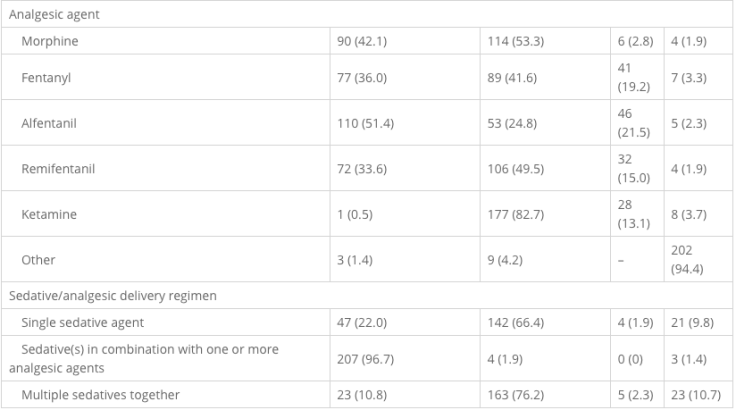
- 51.5% and 42.1% used Alfentanil and morphine respectively
- 39.7 % reported that generally alfentanil was their first choice
- 26.2 % reporting fentanyl as theirs
In combination
- 96.7% reported that they deliver sedative(s) in combination with analgesic(s)
- 47.7 % of units reported cost as very important/important in determining the choice of sedative and/or analgesic agent
- 82.2 % of units reported that the expected duration of sedation/analgesia was very important/important

POINT PREVALENCE SURVEY
- Sedated patients were slightly younger than non-sedated patients (mean age 59.3 years versus 63.6 years) but similar in terms of gender, ethnicity and severe co-morbidities.
- Sedated patients had higher acute severity of illness and were more likely to have been mechanically ventilated (78.4 % versus 43.7 %) during the first 24 h in the unit, and had, on average, been in the unit for a shorter time at the point of the study (mean 6.9 days versus 10.6 days).
- On the day of the study, 12.0 % (n = 29) of the sedated patients were being ventilated via a tracheostomy.
- 14.0 % had received only sedatives
- 17.4 % only analgesics and
- 68.6 % both sedative and analgesic agents.
- A sedation scale/score was recorded for most and the majority used RASS.
The most common combinations of sedative and analgesic agents were propofol combined with either alfentanil or fentanyl. In isolation, propofol was the most frequently used sedative and morphine the most frequently used analgesic.


Do as you say??
Below, we can see what was reported to be done and what was actually done


Interestingly, reported practice did not necessarily reflect actual practice. The same sedation scores were used in the majority, but 94% reported daily sedation holds and only half in the PPS were actually considered.
Propofol is the most used sedative, alfentanil, fentanyl and morphine the preferred analgesics. Most used combinations of both.
Only 57 % of units reported had a written sedation protocol, similar to the findings of a recent Internet-based survey of UK critical care pharmacists in which 55 % of respondents reported use of sedation guidelines. However, this is considerably lower than previously reported in the United Kingdom (perhaps down to reporting logistics).
The RASS is recommended as one of the most valid and reliable subjective sedation scales for measuring depth of sedation. It’s use has increased considerably over the last 5 years. The practice of daily sedation holds is recommended and has been incorporated into the ventilator care bundle. The benefits of minimising sedation are numerous:
- less time on a mechanical ventilator
- fewer complications and reduced length of stay in critical care
We see reports of sedation holds being around 90%+ but only around half (53 %) had been considered for a sedation hold in the previous 24 h, and of these, 77 % had their sedation withheld.
Propofol is popular as ever as 1st choice over benzo’s and the use of the alpha-2 agonist clonidine has increased in the UK, with around one-third of units reporting very frequent/frequent use, whereas use of dexmedetomidine is rare. It seems that uptake of dexmedetomidine in UK critical care has been slow since it was licensed for use in 2011. Cost may be a factor, with clinicians preferring to use established and often cheaper alternatives. We are certainly starting to use it more on our unit, but with the usual forms to fill out to justify the cost!
There seems to be a trend away from morphine toward agents such as alfentanil and fentanyl as the first choice for analgesia, but it is still widely used.
This survey had a 91% response, higher than most before. But, reported practice does not necessarily reflect the reality of actual clinical practice at the patient level. This had a large national survey and PPS, giving it strength.
A major strength of the present study is the combination of a national survey of adult general critical care units and a PPS amongst 51 representative UK ICU’s.
Reported Vs actual practice showed a discrepancy, perhaps for many reasons:
- Lag between a unit policy being initiated and staff at the bedside changing their clinical practice
- Difficulties in applying universal policies on sedation and analgesia to individual patients
- The person completing the survey is influenced by her own practice when reporting unit practice, which may not necessarily reflect that of her colleagues or may not even be in line with the unit policy.
It bolsters the fact that we need to keep tabs on what we say we should be doing (policy) and what we actually are (reality). This needs more of what we all love…audit!!
So….units were perhaps a tad caught out by PPS Vs formal survey, but this is perhaps good in that it reflects relatively unbiased behaviour (no Hawthorne effect!). For me…propofol and alf all the way and sedation holds are vital for our patients. Finally, if we can, we should assess and treat pain FIRST with the analgesia arm of sedation before we add pure non-analgesic sedatives.




















Leave a Reply