Here is my latest trawl of what I considered to be the best of FOAMed at the moment. This is certainly not exhaustive…you can end up like a child in a sweetshop otherwise!
The podcast discussion I had with Jonathan Downham can now be heard by clicking the pic below. This is episode 2 of our fortnightly roundup of interesting papers, blogs and more…
Come August, we have 2 new Social Media in Medicine / research fellows starting with us and they will be a great help in expanding what we do on the site…so a lot more to come! DO have a click around the rest of the site and if you want to contribute, ping me a message!
JW
Click the pic to listen to the podcast in a background window as you scroll through!
Big Papers
Come on WOMAN!!!
There has been a lot of controversy over this one and some slating of the Lancet as well. The trial aimed to ascertain:
- Does the early administration of tranexamic acid (TXA), compared with placebo, reduce death from bleeding in women with post-partum haemorrhage (PPH)?
Tranexamic acid reduces death due to bleeding in women with post-partum haemorrhage with no adverse effects. When used as a treatment for post-partum haemorrhage, tranexamic acid should be given as soon as possible after bleeding onset
Tranexamic acid may be beneficial in reducing the risk of death due to post-partum haemorrhage. The study has some significant methodological limitations, including a change in power calculation (by 5000) and hypothesis change (reduction in mortality from bleeding) after it was commenced after CRASH-2 results
- CRASH-2 demonstrated that TXA reduces all cause death at 4 weeks in trauma patients (Absolute Risk Reduction 1.5%).
On the basis of it being cheap with a good safety profile in this study, consider giving tranexamic early in post-partum haemorrhage. Early resuscitation, management of coagulopathy and surgical assistance with source control, are the most important interventions
Please look at TBL’s analysis below
Surely hypotonic IV fluid is bad…no!??
This crossover study by Manu Malbrain et al consisted of two 48 h study periods, during which 12 fasting healthy adults were treated with:
- Isotonic – NaCl 0.9% in glucose 5% supplemented by 40 mmol litre−1 of potassium chloride
- premixed hypotonic fluid – NaCl 0.32% in glucose 5% containing 26 mmol litre−1 of potassium at a daily rate of 25 ml kg−1 of body weight.
- After 48 h, 595 ml (95% CI: 454–735) less urine was voided with isotonic fluids than hypotonic fluids (P<0.001)
- Isotonic arm had significantly lower aldosterone levels due to inadvertent volume expansion
- Sodium concentrations were higher in the isotonic arm (P<0.001), but all measurements remained within the normal range.
- Potassium concentrations did not differ between the two solutions (P=0.45).
- Chloride concentrations were higher with the isotonic treatment (P<0.001), even causing hyperchloraemia.
- No hypokalaemia or hyponatraemia as result of hypotonic solutions
-
Daily administration of several litres of commonly used i.v. crystalloid fluids will lead to electrolyte–salt overload in surgical patients.
-
This study found that an isotonic crystalloid fluid was associated with less urine output when compared with a hypotonic fluid.
-
More care should be used when prescribing perioperative fluid therapy; this is crucially important when larger volumes are administered over more than 24 h.
Could the answer to sepsis and vasodilatory shock be Angiotensin II??
One we took part in at Northampton. This was a multinational RCT looking at whether a new angiotensin-II analogue drug was effective in the treatment of vasopressor naive vasodilatory shock.
- Encouraging primary outcome results
- time to obtain target MAP was shortened with the drug – 69.9% Vs 23.4%; p<0.001.
- But, no significant difference in mortality seen
- death by day 28 occurred in 46% in the angiotensin II group Vs 54% placebo p=0.12.

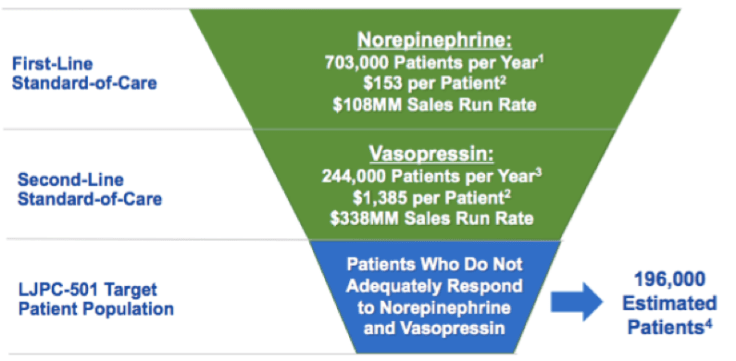


So, it wasn’t powered to detect a mortality benefit, therefore we need a larger RCT powered to do just that. But…will we see the drug coming into usage in 2018?
Care bundles and parts that slow us up?!
The paper from the NEJM below highlights to us again, the importance of rapid diagnosis on low index of suspicion when it comes to sepsis. This large cases series from 1865 hospitals in the US examines the use of a 3 hour care bundle in sepsis.
Interestingly, as you would expect, more rapid completion of a 3-hour bundle of sepsis care and rapid administration of antibiotics was associated with lower risk-adjusted in-hospital mortality. But…delays in initial bolus of IV fluids within the bundle was not! Kind of goes against the 1st Hit principle of R.O.S.E!

Editorials
Invasive Haemodynamic Monitoring…for the tricky ones!!
Although principally about cardiac Catheter indices for the professionals performing them, this is very interesting nonetheless. It gives beautiful tabular definitions of the indices we all consider when monitoring many ICU patients, and some of the more off the wall ones too. The editorial works through the intricacies of vasculoventricular coupling, preload, after load, starling’s law and areas we may need caution over interpretation. One thing’s for certain, if you absorb it all you’ll look like the guru on the ward round when discussing monitoring!
You think you can handle all that is kidney…YES or NO!!
Have a look at the debate below! Very interesting to read both view points and I would love to see this head-to-head at a conference debate. Makes you think though….can we manage this specific organ failure???
Depends on your view-point of course, but Flatten argues we should get nephrologists involved early…after all, we often require renal follow up, particularly after initiation of CVVH and continuation when we can’t wean our patients off the filter.
-
Acute kidney injury is an important issue from the point of view of the patient as well as the healthcare system.
-
Long-term consequences of AKI are frequently underestimated and follow-up of AKI patients may certainly be improved.
-
We are in urgent need of pragmatic and efficient strategies limiting both short-term and long-term consequences of AKI.
-
Early and prolonged nephrology follow-up is a promising non-pharmacological strategy that may increase long-term survival and limit progression toward chronic kidney diseases.

Then there’s always the counter argument!
So here is why we think we may NOT need renal consult on the ICU…

A better approach though, might be to focus on non-recovery. Recovery after AKI is a crossroads for patient outcome. For patients with stage 2–3 AKI, recovery by hospital discharge occurred in 58.8% in one recent large series (more than 16,000 patients) [14]. Patients who recovered by hospital discharge fared much better than those who did not, but the pattern of recovery was also important. The best prognosis was observed with patients who had early (within 1 week) sustained reversal of AKI. More than 90% of these patients were alive at 1 year.
So let’s sit on the fence then…




Click below for KDIGO document in management of AKI
What is meaningful in AKI??!
The above article highlights the problems with research into the ‘golden bullet’ in preventing ESRF after AKI. Classification of AKI is well known, but overall outcomes are always mortality and many trials focus on prevention of AKI. We perhaps need to focus upon CKD as our important end-point, as this is why we get so concerned about AKI isn’t it (obviously mortality aside)? Less focus on biomarkers and more on other adverse events are given important emphasis here.
The composite outcome of death, new dialysis, and worsened renal function, which was defined as a 25% or greater decline in eGFR, constitutes the Major Adverse Kidney Event (MAKE) outcome. MAKE30 is assessed 30 days following AKI diagnosis, and MAKE60 and MAKE90, 60 and 90 days after AKI diagnosis, respectively. MAKE90 may be the most appropriate endpoint because that is typically the time when CKD is diagnosed after AKI.
AKI is a devastating disease, but CKD is worse. The association between AKI and subsequent CKD and the imperfection of current AKI diagnostic criteria and renal damage biomarkers beseech us to include markers of hard clinical outcomes in trials of AKI. Thus, we will solidify the importance of AKI events on patient health and better understand the effects of AKI treatments. The MAKE90 composite endpoint includes persistent renal dysfunction 90 days following AKI, new-onset need for renal replacement therapy, and death, and is therefore a suitable endpoint candidate for this task.
Clinical Stuff
Bloody thinners!!
This is a nice article highlighting a rather grey area of clinical practice frankly. When do you stop those oral anticoagulants, when is it safe to perform anything invasive, do you need bridging therapy and when can you restart them back on what they were on after you’ve done something nasty to them with needles etc! It’s all here, so have a read, or skip to the useful table…it even tells you how they all work!
Out with the old…in with the new?
Diagnostic techniques that do not depend on growth of organisms in culture may offer a distinct advantage over current methods. They allow shorter time to results and detection of non-cultivable microorganisms under antibiotic pressure.
Negatives of BC’s:
- Blood cultures have only 70% specificity, and sensitivity is approximately 10% in suspected bacteremia, 30% in febrile neutropenia, 35% in severe sepsis, and 50% in septic shock. Funny that…we’ve just discussed these statistical measures above!
Negatives of PCR:
- False negative PCR tests can occur by interference with human DNA and the presence of PCR inhibitors in the blood. Furthermore, they can only detect pathogens that are specifically tested for.
But…PCR has a huge specificity advantage when you need results fast, i.e it is better for ruling in than for ruling out infection. So…if we combine the two perhaps, in conjunction with our AST, we may have a better diagnostic accuracy? Let’s face it, even with the important gains we have witnessed with the use of new diagnostic tests, the majority of patients with sepsis will remain undiagnosed for a specific etiology.
A bit about PCR and how it’s done:
Stats!! Stats!! Stats!!
Ever wondered what a ROC is – receiver operating curves help to ascertain the accuracy of a test in clinical practice. This article outlines the use of the ROC with respect to ACS.

Remember:
-
Sensitivity is the proportion of true positives that are correctly identified by the test.
-
Specificity is the proportion of true negatives that are correctly identified by the test.
-
Accuracy is the proportion of correct decisions (ie, true positive+true negative) over the number of total tested.
Also…remember what the Crew at TBL told us about false positives…click the upper pic below:
Other Blogs
Anaphylaxis…myths and mysteries?
This is a lovely read from EMdocs! I particularly enjoyed the parts discussing controversies and it’s always nice to read more on what you think you know about!
Take home points:
-
Severe allergic reactions and anaphylaxis share very similar presentations, are both life threatening, and require immediate lifesaving treatment with epinephrine.
-
Avoid a slow progression to epinephrine by thinking alternative medications (Benadryl, H2 antagonists, steroids) will work. The time of onset of these medications is too long to prevent severe reactions.
-
Consider glucagon for anaphylactic reactions in patients on beta-blockers.
-
The anaphylactic reaction itself is often responsible for coronary vasospasm and arrhythmia Do not avoid giving epinephrine because of these potential reactions.
-
Always prescribe Epi-pen® to all allergic reaction patients. Make sure to counsel these patients on its use in potential future episodes.
Aspirin…get the blue cigar down early??
Salim and the Rebel EM crew talk us through salicylate poisoning..the extremes. Click the pic and read on.
This was a retrospective analysis of a small case series:
- 56 Cases Identified
- 41 of those 56 patients survived (73.2%)
- Of the 15 fatal cases, 11 patients (73.3%) did not receive hemodialysis
- 6 patients did not complete HD, all suffering cardiac arrest
Interesting stuff, as essentially, the metabolic acidosis caused is usually reasonably well dealt with by normal physio;logy..profound and excessive hyperventilation tom eradicate volatile acid in the form of CO2. But, the ventilator removes that physiological hammock, as typically,you can’t match this with the ventilator. So, your patient effectively requires dual organ support at least; filtration AND ventilation to overcome the nasty side effects to bridge them towards survival.
‘Survival was decreased in these patients if hemodialysis was not performed. Mortality increases with the measured serum salicylate level. Timely hemodialysis for intubated salicylate overdose patients decreases mortality.”
INFOGRAPHS
Adult ICU pre-Intubation Checklist (Courtesy of Alfred ICU)


Approaching the Oedematous intubated airway!

POCUS

This playlist has to be seen!











































Leave a Reply