There has been a lot of action on the POCUS front, as well as some of the usual fabulous and bountiful FOAM Tweets this week and last.
We have had a lot of activity over the last couple of months and a massive thanks to you all for supporting us. We are up to around 1500 followers now, which is more than I could hope for at this stage! I hope to bolster the site with more over the next month so watch this (web)space!
Happy weekend folks…enjoy the read and remember, some of the Twitter screenshots are clickable!
History in Action
Have a read of this fabulous article about the evolution of blood gas measurement. It discusses the major revolution in technology after the great polio epidemic, as well as what the pioneers did very early on the path to discovery.
The Bottom Liners
The Bottom Line crew looked at 2 big papers this and last week. The first:
The trial used HFNC immediately post op in order to see whether it prevented hypoxia versus standard O2 therapy in abdominal patients. They conclude that even though the trial did not show major benefit, selective and patient specific usage still helps. We have probably all seen this in reality….but often, trials do not reflect reality.
See also the FLORALI trial.
The second:
This paper was another hopeful to address the continuing panic state we all seem to get into regarding post contrast nephropathy. NAC, bicarb etc etc all tried to little avail! In this study they aimed to ‘hydrate’ patients with N saline prior to getting the contrast to see if the effect on CIN was a positive one or not. It appeared that:
no hydration was non-inferior to hydration in the prevention of contrast induced nephropathy. Hydration is more expensive and can cause problems in itself.
So hydration prior to contrast administration may not be necessary in all patients previously thought at risk to develop CIN. But, we should still hydrate higher risk patients if they have haemodynamic compromise, are on nephrotoxic drugs and are about to receive high contrast concentrations. Those with poor GFR <30 are at particular risk so should be rehydrated.
General Papers
Fluid challenges in the ED…are a challenge!!
The haemodynamic dilemma in emergency care: Is fluid responsiveness the answer? A systematic review
Seems there is no consensus, but this search of 249 potential studies pulled 3 total worth a look. Interesting points on the agreement on what is ‘fluid responsive’…used to be >20% response…now we seem to have loosened a bit to >15% as being acceptable on SV / CO.
What we can learn from Combat!
Fluid resuscitation in haemorrhagic shock in combat casualties
I love the papers that come out of the military setting. They get the chance to look at the fittest of the fit and extrapolate information based on model physiology. They also seem to have the money and resources to do so, as well as different ethical thresholds. This paper looks at the best resuscitation strategies in trauma settings.
Do you know what Kounis Syndrome is….watch that sushi and Gelo!!
Have a read through this rather interesting paper on Kounis Syndrome. Seems it may be rather un-diagnosed!

Lactate…again!
Lactic acidosis: an update – the most talked about biochemical! This article highlights some of the key trials where this ‘biomarker’ was used as a resuscitation guide. There is also a lot of the historical stuff in there which nicely mirrors the history article at the top of this page. Part of the article actually debates whether we should be chasing this as a resuscitative goal!


Biomarkers won’t highlight the killer!
Cardiac troponins and mortality in type 1 and 2 myocardial infarction. This is an interesting paper, which for starters raised my awareness of M.I and the fact there are various subtypes with different mortalities. The only thing is, the troponin value of the M.I subtype with the greater mortality is in fact lower.
Paper of the week!
PPC’s … do all you can to avoid them!
This paper from the BJA really is worth a read. It discusses the thing we all want to avoid for our patients…Post op Pulmonary Complications or PPC’s. Reading this through, it makes one realise the vital role of the anaesthesiologist in providing life and physiological support. The discussions regarding pre-operative measures to minimise it and also discussions regarding PEEP / Low Vt ventilation, smoking cessation and other co-morbidity optimisation are poignant.
Case Report of note!
Here is a nice little case report of a lady presenting with ACE induced airway oedema. This is a great example of what US can show us. This may be a great way to avoid immediate crash intubation, but will require significant confidence, skill and experience to hang your hat on!

ED/EM Stuff
Shock em’……perhaps block em’!
A great blog here on pharmacological methods of VT eradication. I liked this as it offers more to the armoury than just the mirror signal manoeuvre amiodarone.
Sit up and hold your head high!
Head-Elevated Patient Positioning Decreases Complications of Emergent Tracheal Intubation in the Ward and Intensive Care Unit. This nifty paper looked at what we all know we should do, get them into the ‘sniffing the morning air’ position. However, they looked at the Bed-Up-Head-Elevated Position for Emergent Intubation or B-U-H-E.

“Placing patients in a back-up head-elevated position, compared with supine
position, during emergency tracheal intubation was associated with a reduced odds of airway related complications.”
It’s not just DKA!
So here is a lovely article to look at from the emDocs. They discuss the effects alcohol ketoacidosis has on your metabolic state….similar to DKA. Worth a read and another cause of that good old abnormal anion gap acidosis we bang on about!
Can’t get rid of that VT!
Another great piece by the emDocs on VT. Various management options given here, all of which are really helpful. The temptation is always Amiodarone for most arrhythmias these days…but read this REFRACTORY VENTRICULAR TACHYCARDIA: APPROACH TO MANAGEMENT article to widen your approach.
Cardiovascular
Reach for the norad then?!
The paper below raises more debate about the so called life-saving usage of that good old minijet drug we all love(d)!
“Among vasopressors and inotropes, adrenaline was independently associated with 90-day mortality in cardiogenic shock. Moreover, adrenaline use was associated with marked worsening in cardiac and renal biomarkers. The combined use of noradrenaline with either dobutamine or levosimendan appeared prognostically similar”.
Echo Echo Echo!
Don’t lose them…tap it out!
Have a look at this section from the crew at ultrasound of the week. They discuss pericardial effusion and tamponade state. Brilliant images and info graphs as well.
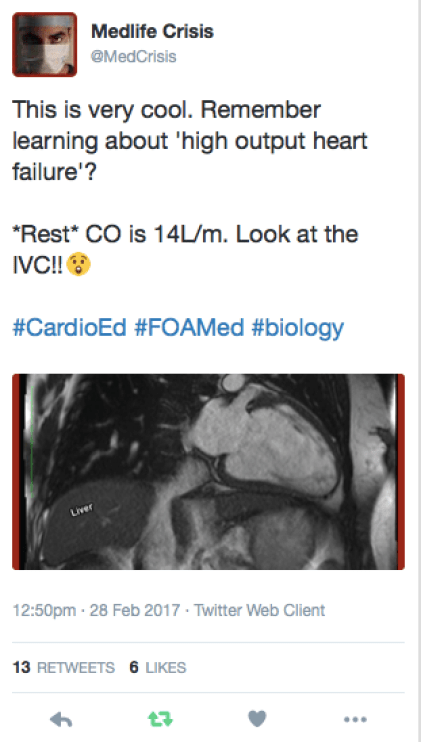
#LEARNPOCUS #POCUS
Another article in support of usage of POCUS in rapid diagnostics.


Medicine
Manage those sugars!
A lovely little snippet here from EmNote. Management of T2 diabetes. Quick, easy to read and to the point!
HAP, VAP, CAP….??!!!$%&&%
Here is a nice article clearing up the confusion between acronyms relating to pneumonia. This condition still counts for the majority of sepsis related deaths around the world…so use CURB-65 and appropriate antibiotics as soon a you can.
Coffee Time Game!
Click here to access the Sepsis game…UK relevent! Nice little reminder of the fight we have to treat and understand this killer condition. Click the image:
Fantastic Tutorial series on airway management
Click here to got through POCUS for the airway











Infographics

JW March 2017






































Leave a Reply